LOS ANGELES — Both primary efficacy endpoints were met in the phase 3 ACHIEVE I trial, a randomized controlled study comparing the novel oral calcitonin gene-related peptide (CGRP) receptor antagonist ubrogepant (Allergan) vs placebo for acute treatment of a single attack of migraine, report researchers.
Findings from ACHIEVE I, which included more than 1300 patients in the intent-to-treat analysis, showed that significantly more of those who received 50 mg or 100 mg of the study drug achieved “pain freedom” 2 hours after treatment (in 19% and 21%, respectively) than those who received matching placebo (12%).
Greater percentages of both dosing groups also achieved absence of migraine-related most bothersome symptoms (MBS), including photophobia, phonophobia, and nausea, vs placebo (in 39% and 38% vs 28%, respectively).
Although the most common adverse events (AEs) were nausea, somnolence, and dry mouth, all were reported by fewer than 5% of the participants receiving ubrogepant.
“I think the number 1 takeaway is that we met the primary endpoints of decreasing headache pain and symptoms at both doses,” said lead author, Joel M. Trugman, MD, associate vice president in clinical development in Allergan’s research and development area, at a press conference ahead of his presentation here at the American Academy of Neurology (AAN) 2018 Annual Meeting.

Dr Joel M. Trugman
He later told Medscape Medical News that he believes the novel medication “holds great promise for migraine patients.”
Chair of the meeting’s scientific committee, Natalia S Rost, MD, MPH, director of the Acute Stroke Service at Massachusetts General Hospital and associate professor of neurology at Harvard Medical School, Boston, noted that she would have preferred seeing the study comparator be something other than placebo.
However, she added that research into CGRP-targeting treatment for acute migraine, especially at the phase 3 level, is welcomed.
“This step showed that it’s more effective than placebo. Next step will be to prove that it’s more effective than a competitor,” Rost told Medscape Medical News.
“Getting at” Key Molecule
CGRP “is highly expressed in pain-sensitive trigeminal sensory neurons which innervate the dura and meningeal blood vessels [and] CGRP is pathologically released during the headache phase of migraine,” write the investigators.
Ubrogepant “is getting at one of the key molecules in migraine pathophysiology,” added Trugman.
Two phase 3 trials, ACHIEVE I and ACHIEVE II, were created to assess this drug for the acute treatment of migraine. Whereas ACHIEVE I evaluated 50-mg and 100-mg doses, ACHIEVE II is assessing 25-mg and 50-mg doses.
Results from ACHIEVE II are expected to be released before July 1 of this year, reported Trugman. He added that, on the basis of the findings from both trials and a few longer-term safety trials, the manufacturer hopes to submit a new drug application to the US Food and Drug Administration during the first part of 2019.
As reported at the time by Medscape Medical News, positive results from a phase 2b trial in 640 patients assessing five different doses of the study drug vs placebo were presented at the American Headache Society Annual Scientific Meeting in 2016.
In this present analysis, the investigators note that for many patients with migraine, there are no optimal acute treatments because of “inadequate efficacy, tolerability issues, and contraindications.” This includes triptans, which should not be used in patients with cardiovascular disease.
“There are a limited number of options for patients with migraine, so a novel, fast-acting therapy with a clear, migraine-specific mechanism of action that is well tolerated is going to bring options,” said Trugman.
Primary, Several Secondary Endpoints Met
In ACHIEVE I, the 1672 participants (87.5% women; 82.4% white; mean age, 40.7 years) were randomly assigned to receive placebo (n = 559) or ubrogepant at the lower (n = 556) or higher (n = 557) dosages.
All of the patients had a history of migraine, with and without aura. They had up to 60 days to treat a single migraine attack with moderate-to-severe headache pain intensity with their assigned therapy. At baseline, 63% reported moderate pain and 37% reported severe pain. In addition, 11% had moderate-to-high cardiovascular risk at baseline.
A total of 1436 of the participants were included in the safety-assessing analysis, while 1327 were included in the modified intent-to-treat efficacy analysis.
Photophobia was the MBS reported at time of treatment (by 56.4%), followed by phonophobia (22.3%) and nausea (20.9%).
Both co-primary endpoints, evaluated 2 hours after initial treatment, were greater in both ubrogepant groups compared with the placebo group:
Secondary endpoints showed that 61% of each dosing group achieved pain relief at 2 hours vs 49% of the placebo group (adjusted P = .002 for both comparisons); 36% and 38%, respectively had sustained pain relief between hours 2 and 24 hours vs 21% (P = .002).
Significantly more members of the 100-mg group also had sustained pain freedom at 2 to 24 hours (15.4% vs 8.6%, P = .002) and absence of photophobia at 2 hours (45.8% vs 31.4%, P < .0001).
In addition, the study drug “was well-tolerated with no identified safety concerns,” reported Trugman, adding that “the AE profile was similar to placebo.”
Safety Data
In the ubrogepant 50 mg and 100 mg and placebo groups, 9.4%, 16.3%, and 12.8%, respectively, reported an AE. Also, 5.8%, 12.0%, and 8.5% reported a treatment-related AE.
Nausea was reported by 1.7%, 4.1%, and 1.6% of the groups, respectively; somnolence by 0.6%, 2.5%, and 0.8%; and dry mouth by 0.6%, 2.1%, and 0.4%.
Among the five serious AEs reported within 30 days were two reports of appendicitis and one report each of pericardial effusion, spontaneous abortion, and seizure.
Only the seizure was considered to be treatment related. A generalized seizure occurred 6 hours after a 44-year-old woman took ubrogepant at the 100-mg dose. “Alprazolam (benzodiazepine) withdrawal [was] considered a possible etiology,” write the investigators.
Regarding liver safety, there were six instances of having at least three times the upper limit of normal alanine aminotransferase or aspartate aminotransferase elevation: one within 7 days of treatment exposure and the others at the 1-month safety follow-up. Of these, four instances occurred while the patients were receiving ubrogepant but were adjudicated as “unlikely” to be related to study medication. The remaining two cases, one during receipt of the study drug and one during receipt of placebo, were adjudicated as “possibly related” to treatment. None were found to be “probably related” to treatment.
“The liver safety data from this study do not suggest any signal of hepatoxicity for ubrogepant,” write the researchers.
During a question-and-answer session, Trugman was asked whether pregnancy or potential pregnancy was assessed, and he replied that that subgroup was excluded from the trial.
“These are small molecule, orally available drugs that differ very much from the monoclonal antibodies that are being developed for prevention. These drugs get rapidly absorbed and, basically, they’re gone from the system in 24 hours. In that sense, they’re safer than having a long term monoclonal,” he said.
“But in general, we would not recommend this” for patients who are pregnant, he added. “That would be something that would be further evaluated, and if gets to the point, I’m sure it’ll be labelled properly.”
Overall, “this is cutting edge, innovative, hopefully valuable medication. And it’s something that the migraine community has been looking for a long time,” said Trugman.
A “First Step”
It was during the press conference, which she moderated, that Rost first voiced her concern with the study’s design.
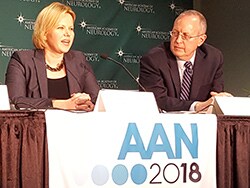
Dr Natalia S Rost (left) and Dr Joel M. Trugman (right)
“These trials are done in large part for regulatory purposes, and the FDA wants to be sure that our drug is effective and that it’s better than placebo,” replied Trugman. “That’s their main task. They want to see statistical significance and clinically relevant improvements.”
“I think it would be raising the bar a little bit in terms of comparing it with the competition,” Rost answered back.
She later told Medscape Medical News that although comparing the drug with placebo wasn’t ideal, she did choose the study as one of her top picks of the meeting.
“That’s mostly because of the development of a new paradigm in treatments. The more diversity there is in the way the science develops, the more hope we have for the development of efficient treatments,” said Rost.
“This is a first step [for the investigators]. It’s like a base one; they have to score with the FDA and they have to show efficacy. The next step will be: Now that you’ve shown that you’re better than a glass of water, how about we compare to aspirin or ibuprofen or acetaminophen,” said Rost.
She noted that she’s envisioning that before this drug is allowed into the markets, it has to prove that it’s more effective than triptans. “The effectiveness is going to need to bring the punch with it and not just the promise.”
Rost added that if ubrogepant is later proven to be more effective than triptans over the long run, “I wonder if there will be a reprieve for those who have contraindications to triptans. If so, I wonder if this will be another niche that could benefit from it.”
“The more interest in disease biology that’s out there and the more effort into the development of multiple medications, the more chance we have to provide relief,” she concluded.
The study was funded by Allergan. Trugman reports holding stocks and/or stock option in Allergan. Rost has received personal compensation for consulting, serving on a scientific board, speaking, or other activities from Broadview Ventures, Covance Inc, Merck and Co, Omniox, and Sanofic Genzyme and has received personal compensation in an editorial capacity for UpToDate and Current Treatment Options in Cardiovascular Medicine.
American Academy of Neurology (AAN) 2018 Annual Meeting. Emerging Science Abstract 008. To be presented April 24, 2018.
Follow Deborah Brauser on Twitter: @MedscapeDeb . For more Medscape Neurology news, join us on Facebook and Twitter .
Tidak ada komentar:
Posting Komentar