Rates of antibiotic-resistant infections have roughly doubled since 2002, and the cost of care now tops $2 billion per year in the United States, researchers report in an article published online March 22 in Health Affairs.
Estimating the prevalence of these cases was complicated by the fact that only 12% of the cases were correctly identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes, write Kenneth E. Thorpe, PhD, the Robert W. Woodruff Professor and chair of the Department of Health Policy and Management, Rollins School of Public Health, Emory University, Atlanta, Georgia, and colleagues . To correct this, they suggest that payers such as Medicare and Medicaid offer increased reimbursement when coding indicates treatment for an antibiotic-resistant infection.
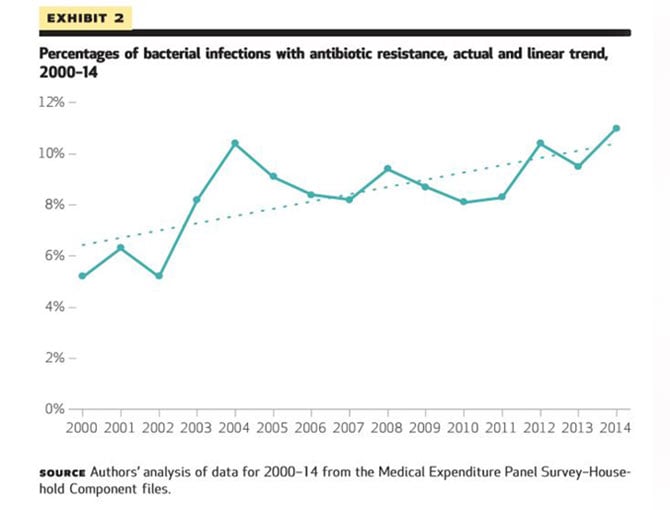
In what the authors say is the first national estimate of the costs for treating antibiotic-resistant infections, Thorpe and colleagues found that while the overall number of bacterial infections remained relatively constant between 2002 and 2014, rising from 13.5 million to 14.3 million annually, the proportion that were antibiotic resistant rose dramatically, from 5.2% to 11.0%.
The mean costs of treatment were $1394 for patients with a drug-susceptible infection and $3698 for those with drug-resistant infections, representing an increase of 165%. However, in a multivariable regression analysis that adjusted for multiple factors, including comorbidities (which were more common among patients with antibiotic-resistant infections), the incremental cost was $1383.
In 2014, with more than 1.5 million cases of drug-resistant infections, the incremental cost amounted to an additional national treatment cost of approximately $2.2 billion.
The authors note that this is almost certainly an underestimation of the overall cost because the analysis did not include data for institutionalized patients, such as those in nursing homes, other long-term care facilities, prisons, and military or Veterans Affairs facilities, all of which typically have higher rates of antibiotic-resistant infections. Nor did the analysis include children, “who are the primary carriers of methicillin-resistant Staphylococcus aureus and pneumococcus in the community,” they write.
Moreover, the authors restricted their cost analysis to clinical expenses. “We did not include indirect societal costs, opportunity costs of not being able to perform certain procedures because of the presence of the infections, the costs of morbidity and mortality attributable to them, or other spending for infection control and antibiotic stewardship.”
The authors used data from the Medical Expenditure Panel Survey (MEPS) for the years 2002 through 2014 to estimate the incremental healthcare costs of treating a resistant infection in an adult patient, as well as the total national costs of such treatment.
They identified treatment-resistant infections by using ICD-9-CM codes, as well as evidence of treatment failure, defined as use of two or more therapeutic subclasses of prescription antibiotics to treat a bacterial infection.
Relatively few of these resistant infections were identified by using diagnosis codes. “Overall, 88 percent of antibiotic-resistant infections were identified by our second criterion, treatment failure, while only 12 percent were identified by ICD-
9-CM diagnosis codes,” Thorpe and colleagues write. This suggests that there are nearly nine antibiotic-resistant infections for every one identified by ICD-9-CM codes.
The authors emphasize that underuse of codes hampers infection detection and surveillance, as well as impeding large-scale research efforts to uncover the infections’ true prevalence and burden.
For clinicians, these findings also have financial implications. The strong correlation between administrative diagnostic coding and payment, plus widespread undercoding of antibiotic-resistant infections, “creates a strong disincentive for physicians to specialize in infectious diseases and for insurers to reimburse providers for treating them,” the authors write.
The study was funded by a restricted grant from Merck and Co. to the Partnership to Fight Chronic Disease, which Thorpe chairs. The authors have disclosed no other relevant financial relationships.
Health Aff. Published online March 23, 2018. Abstract
For more news, join us on Facebook and Twitter
Tidak ada komentar:
Posting Komentar